
LET'S TALK ABOUT IT
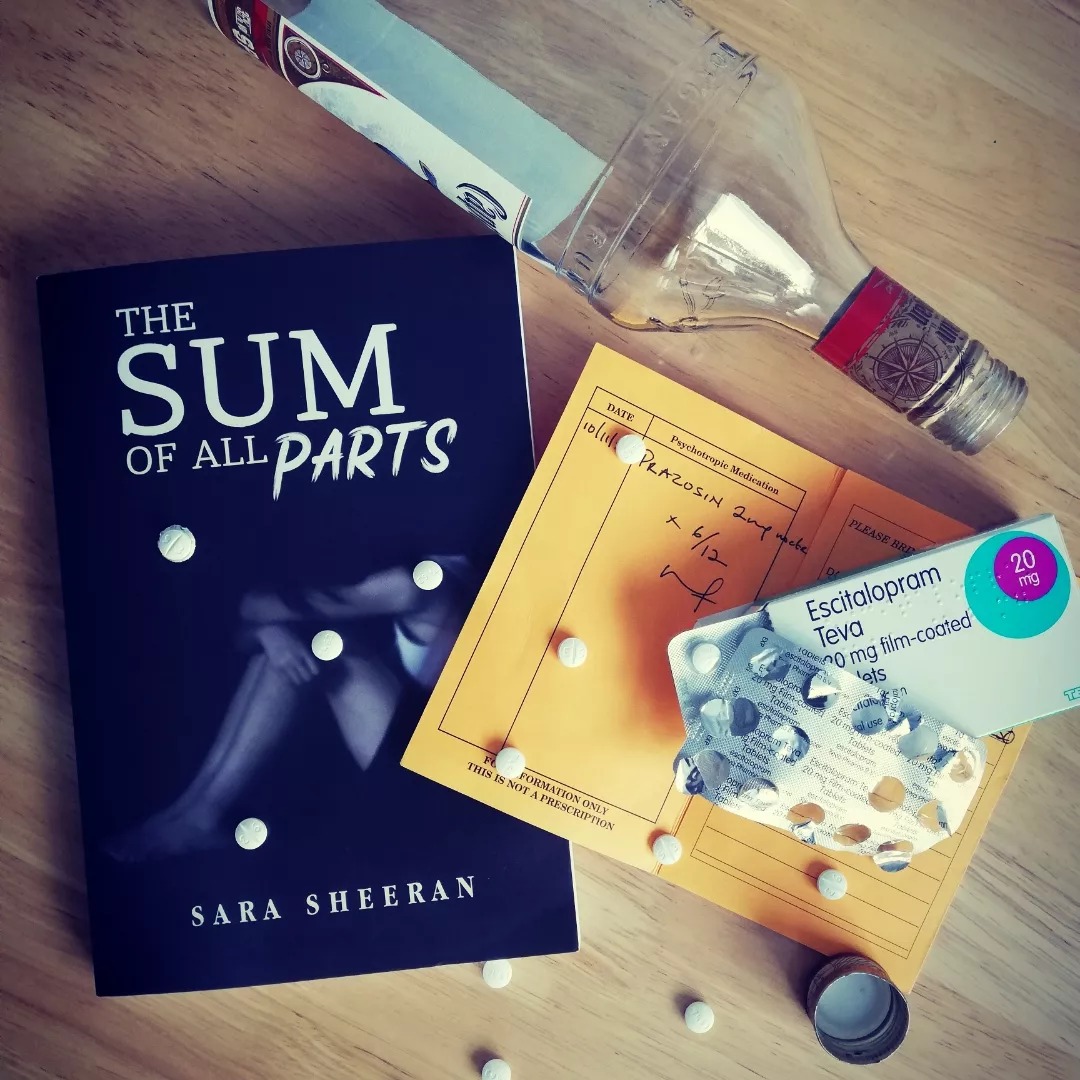
Today, 10th September, is, as it has been since 2003, World Suicide Prevention Day. A day to create hope through action and to remind ourselves that suicide can be prevented. As my book The Sum of all Parts deals with depression, anxiety, post traumatic stress disorder (PTSD), and suicide (all areas I researched thoroughly - my browser history made for uncomfortable reading) I thought today would be a good day to discuss that sticky subject that is mental health.
I don't know where you are in the world as you read this blog, but I am in Ireland - Carlow to be precise - and I'm afraid to say that our mental health provision leaves a lot to be desired. When researching The Sum of all Parts I spoke to a prominent consultant psychiatrist for the Health Service Executive (HSE) - I shan't give any more detail than that - and he complained of being over-worked and under-staffed to the point of not being able to provide his patients with the treatment that they needed. I also spoke to someone with depression and PTSD who, at the time of writing my book, was lucky to be receiving Cognitive Behavioural Therapy (CBT) alongside drug treatment. Fast forward to this spring when I caught up with this person: she had missed an appointment with the mental health unit in the summer of 2022 due to having COVID but rang and the secretary said a new appointment would be arranged. She heard nothing for months, but thought nothing of it - this was not unusual. By spring 2023 she had deteriorated and was having suicidal thoughts. She rang the mental health unit to chase up the appointment and was told that she was no longer a patient as she had failed to attend her last appointment. She explained that she had rung, that she was told a new appointment was meant to be sent out to her, but to no avail. She could not be seen, would not be seen. Instead she was advised to head to Accident and Emergency. A good idea? Let's talk logistics: A&E is nearly 40km away, and if you don't drive - like this woman - it means a train or a coach and then either a cab or a half hour walk. On top of that, with no GP referral it would cost 100 euro. On top of that, we're talking about sending someone with depression, PTSD, and suicidal thoughts on that journey. She didn't go - she couldn't. Instead she went to her GP and was re-referred to the mental health unit and to Counselling in Primary Care (CIPC). As of today she still hasn't heard from the mental health unit and although she was registered with CIPC within weeks, no counselling date has been given. But hey, it's all ok isn't it? I mean, once a year we 'create hope', or at least awareness, if not through action but by putting up posts on social media or by writing blogs like this which if I'm lucky will be read by a few people; we participate in sponsored walks to assuage our guilt and/or to feel better about ourselves; and, my personal favourite, we paint murals - because spending money on murals is far more important than providing Ireland with psychiatrists, psychologists and therapists.
Let's back this up with some facts: Ireland has one of the highest rates of mental health illness in Europe, ranking joint third out of 36 countries surveyed in the annual Health at a Glance report. In 2016 about 18.5% of the Irish population was recorded as having a mental health disorder eg anxiety, bipolar, schizophrenia, depression and/or drug or alcohol use (www.irishtimes.com). That was 2016, I hear you cry, surely things are better now - we're more aware, we have wall murals. Ok. Let's take a look at the gov.ie health survey of 2021. This showed a 30% worsening of mental health. Negative mental health was measured using the Mental Health Index-5 (MHI-5). The average MHI-5 score in 2016 was 81.2. In 2021 that had dropped to 76.0 in the Healthy Ireland survey.
Still not convinced that the murals, the lapel ribbons, the special days, the sponsored walks aren't improving Ireland's mental health and preventing suicide? Let me take you to a TASC (the think-tank for action on social change) report of March 2023 - report which involved interviews with representatives from the mental health sector, including doctors and psychiatrists, with people working in advocacy and third sector organisations. The report found that Ireland state services are 'hospital centric and lack primary mental health services.' It also found that 42% of Irish population met the diagnostic requirements for at least one mental health disorder and that more than one in ten adults had attempted suicide. The report welcomed the recent development of on-line mental-health and therapy delivery, but it warned that Ireland is 'not a panacea for mental health services.' It stated that there is a lack of access to certain key services in Ireland 'such as help for those experiencing a mental health crisis or emergency' , and surprise surprise, that spending on mental health is relatively low.
'We will see you back here in three months, and in the meantime, any problems - if you feel overwhelmed - call this number,' he underlines a telephone number on the appointment card. 'We are here Monday to Friday, nine to five.'
She wonders what she is supposed to do out of office hours or on weekends. Maybe you're not allowed to be unwell or suicidal during these periods. THE SUM OF ALL PARTS, SARA SHEERAN
A recent article in The Irish Times also reports on a growing mental health crisis in Ireland among young adults and children. Between 2020 and 2021 demand for Child and Adolescent Mental Health Services (Camhs) increased by 33%, while simultaneously seeing a 21% increase in cases. Like my source who is waiting to be seen by the mental health unit and CIPC, the waiting list is also outrageous for children- they are experiencing a 2 year wait for an appointment. In February 2023 4434 children were waiting to access services, up from 2755 in December 2020. According to sources working in general practice cited in this article, this situation means many doctors feel that the only option available to them when a child presents with mental distress is to prescribe anti-depressants - and I would argue that the same can be said with doctors and adult patients given the decline in mental health, the increase in patients and the lack of resources and staff. But back to children and young adults and the subscribing of anti-depressants as a quick if temporary fix, the Health Service Executive (HSE) figures back this up: 15,113 prescriptions for anti-depressants were issued to children aged 15 and younger in 2022, up 130% on the 6541 issued ten years previously. Many questions need answering here - why are our children suffering from mental health issues? What can we do to help? Are anti-depressants the answer? For me, as far as medication goes - and please note that I am no expert nor am I advocating against ant-depressants - anti-depressants will not solve mental health issues, only talk therapy (such as CBT) can help to do this, and therefore medication should be used in conjunction with this and not solely relied on. It is an area I touched on in The Sum of all Parts, with The Patient involved in CBT and on anti-depressants with a view to being weaned off the medication if CBT was helpful. You may recall in the book - assuming you've read it, if not skip this bit and go buy a copy! - the patient refuses to take pregabalin:
At her doctor's surgery a little while later, she cautiously her new appointment card which lists her new prescription, to the receptionist. She feels awkward and embarrassed, now everyone knows that she is mentally unstable. The card made it too real, she was officially insane.
'I need these prescriptions please,' she says. 'But not the pregabalin. I'm not taking that.' THE SUM OF ALL PARTS, SARA SHEERAN
A contradiction you say? After all I've just advocated using medication in conjunction with talk therapy. Well, let me quickly explain. I did my research for The Sum of all Parts like I said, and I researched medications, and pregabalin (sold under the brand name lyrica among others and known on the street as 'buds' due to there colour and the similarity to a certain alcoholic beverage) is ananticonvulsant, analgesic and anxiolytic medication used to treatepilepsy, neuropathic pain, fibromyalgia, restless leg syndrome, opioid withdrawal and generalized anxiety disorder. It appears to be a wonder drug and it is one that, from my research, appears to be handed out by certain practitioners like sweeties to those with mental health issues and any talk therapy is disregarded. The problem I have with it are its many common side effects which includeheadaches, dizziness, sleepiness, confusion, trouble with memory, poor coordination, dry mouth, problems with vision, and weight gain - I myself have witnessed many people on this drug and I can only describe them as virtual zombies.Serious side effects may includeangioedema, drug misuse and an increased suiciderisk - yep that's right, give the patient with a mental health issue a drug that increases their risk of suicide. And please don't think I'm being neurotic over this particular drug - go search online, read the countless articles from official sites warning against it, condemning it. Even the HSE has a PDF (Prescription writing, dispensing and storage requirements for Schedule 3 and Schedule 4 Part 1 drugs (hse.ie)) about the correct prescribing of the drug:
Vigilance is required when prescribing pregabalin due to the risk of dependence and the potential for illegal diversion and medicinal misuse.1
The relaxant and sedative effects of pregabalin make it desirable for use outside of its three licensed indications.
2 Patients misusing pregabalin describe improved
sociability, euphoria, relaxation and a sense of calm.3 Pregabalin may be used to enhance the euphoric effects of other drugs such as opioids.2
Drug-related death figures compiled by the Health Research Board have shown an increase in deaths where pregabalin was implicated, from 14 in 2013 to 45 in 2017.4
The Irish Medical Council advise all doctors prescribing pregabalin to follow best practice guidelines and to only prescribe when absolutely required (September 2019). HSE
So yes, medication has its place when treating mental health issues but I believe that we, as patients, shouldn't just blindly take anything a doctor prescribes, and when it comes to mental health some form of talk therapy is vital. In the Irish Times article I referred to earlier, Professor McLachlan of Maynooth University also supports this saying that if children are put on anti-depressants "they should only be on a short-term basis and should always be accompanied by a therapeutic intervention which is not drug based." I would go further and say that anyone with mental health issues, irrespective of age, needs access to therapeutic interventions: medication alone is not the answer.
It would be fair to say that Ireland is facing a crisis in terms of mental health. More and more people are struggling with mental health issues and the mental health provision we currently have just isn't able to cope. Wall murals and good intentions just aren't enough. Like the slogan for World Suicide Prevention Day says - we need to create hope through action. That action can start with the government increasing its spending on mental health so that there are enough psychiatrists, therapists and other professionals to meet with demand. In the meantime, remember we are our own worst enemy and our negative thoughts - if left unchecked - can do serious harm. So find someone to talk to - a friend, a family member, a doctor or therapist; if feeling stressed or anxious try mindfulness exercises, yoga, take a walk or go for a run - do whatever calms you. Find a way out of your emotional brain and into the rational.
Mind yourself.
For more information and support:
RTÉ.ie/news/2023/0323/1365790-mental-health/
www.mentalhealthireland.ie
www.mentalhealthreform.ie
www.shine.ie
www.aware.ie
HSE: Your Mental Health Information Line, freephone 1800 111 888
Pieta 014585490
www.samaritans.org/samaritans.ireland freephone 116 123, email jo@samaritans.ie
Post Views : 160